Tuberculosis (TB) remains one of South Africa’s toughest public health problems. Dr Stephan Schoeman, under the supervision of Professors Willie Perold and Gerhard Walzl, designed, built, and tested a portable electrochemical biosensor that promises quicker, easier screening, especially where laboratory resources are scarce.
Why Faster TB Screening Matters
The World Health Organisation estimates that 10.6 million people developed TB in 2021, with 8.2 million new people diagnosed in 2023. South Africa recorded one of the highest incidence rates worldwide. Yet hundreds of thousands of cases still go undetected each year. Current clinic-based tests rely on sputum samples, expensive instruments, and skilled technicians—conditions that are difficult to guarantee in many primary-care settings.
To close that gap, the WHO has issued target product profiles calling for low-cost devices that can detect TB from markers in blood, urine, or breath. That challenge inspired Dr Schoeman’s research: the design of a miniaturised, disposable biosensor able to quantify TB-linked proteins at the point of care.
The Research Objectives
In light of the above, the research team set five objectives:
- Review the landscape: Map existing TB biosensors and electrochemical detection techniques.
- Analyse a commercial sensor: Benchmark sensitivity, stability, and ease of manufacture.
- Prototype iteratively: Test materials, electrode layouts, and bonding methods across multiple design cycles.
- Prove the concept: Use the final build to measure a clinically relevant biomarker, C-reactive protein (CRP).
- Chart the road ahead: Outline improvements and broader applications.
Building the Device—One Prototype at a Time
Early designs borrowed ideas from glucose test strips and lateral-flow assays. Carbon nanofibres were selected as the electrode material for their high surface area and biocompatibility. A porous membrane was sandwiched between two working electrodes, creating a control channel that validates every test, much like the control line on a home pregnancy test.
Six successive prototypes tackled manufacturability hurdles such as reliable micro-patterning, fluid routing, and encapsulation. The final version, dubbed Sensor M, integrated all lessons learned:
- Four-electrode cell: Two working electrodes (test + control), one reference, one counter.
- Plug-and-play reagent layer: Pre-coated with capture antibodies specific to CRP.
- Disposable cartridge: Fabricated entirely with equipment available in the Department of Electrical and Electronic Engineering.
Sensor M detected CRP across an impressive 10 ng/mL – 1 pg/mL range—a thousand-fold span that covers concentrations relevant to TB triage. The built-in control electrode confirmed assay validity in every run, boosting confidence in field conditions where repeat testing is costly.
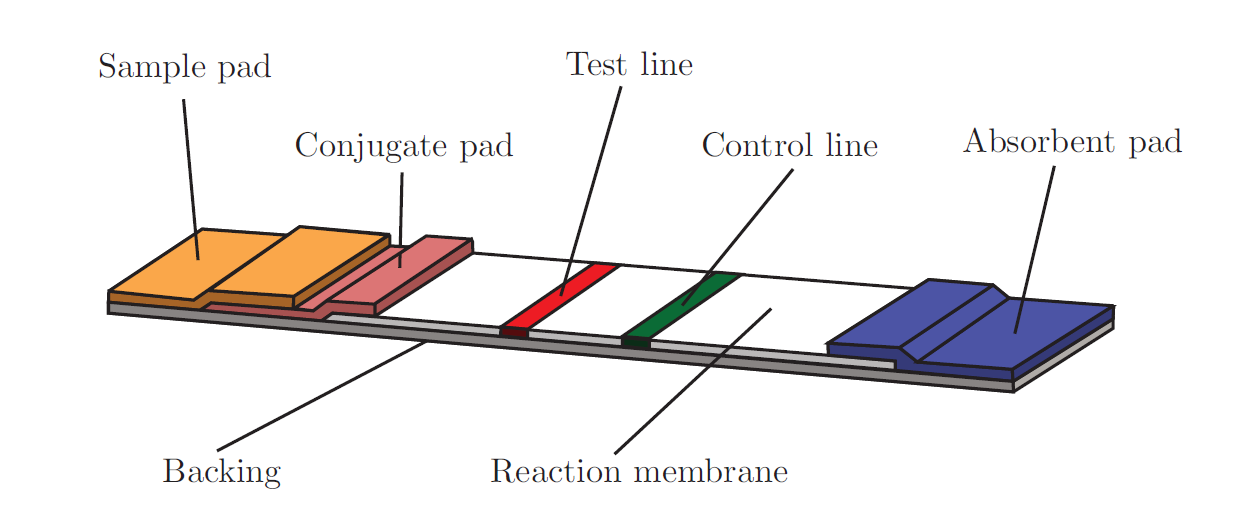
Figure 1: Components of a lateral flow device include a sample pad, conjugate pad, test line, control line, absorbent pad, reaction membrane, and a backing card.
Why it Matters
The sensor delivers results within minutes because it works without culture growth or complex optics. Its credit-card footprint fits neatly into mobile clinics and community screenings, while carbon nanofibre electrodes and off-the-shelf membranes keep materials affordable. Just as importantly, the underlying platform can be adapted to detect other diseases—HIV, sepsis, or even environmental toxins—making it a truly scalable solution.
What’s Next?
- Clinical validation: Partnering with local health centres to compare sensor readings against gold-standard laboratory tests.
- Manufacturing scale-up: Automating electrode deposition to cut unit costs further.
- Multiplexing: Expanding the cartridge to read several biomarkers simultaneously, sharpening diagnostic accuracy.
“Our goal was never a lab curiosity,” says Dr Schoeman. “We wanted a tool nurses can use during a single consultation, allowing patients to start treatment before they leave the clinic.” This project exemplifies how engineering research can accelerate public-health breakthroughs—one prototype, one electrode, and ultimately one patient at a time.
Download and read the full research: https://scholar.sun.ac.za/items/bdfb6c5d-7731-4959-8b18-11ce9a886c1e